ENDOTHELIAL PROGENITOR CELLS
Description of endothelial cells, their development and their progenitor cells incl. methods of isolation and usage in stem cell therapy.
1. ENDOTHELIAL CELLS
Endothelial cells line blood and lymphatic vessels. Endothelial cells prevent blood clotting; their surface is charged negatively due to 10 nm glycosaminoglycan layer (that repels thrombocytes). Endothelial cells are flattened cells sending thin lamellar protrusions through which gas exchange occurs – cell size is 30 x 12 x 0.3 μm. Endothelial cells are usually classified as single squamous epithelium. Nevertheless cell shape can differ in some organs – in venous sinusoids of the spleen they have characteristics of spindle-shaped cells; in postcapillary venules of the lymph node they are described as high cuboidal endothelial cells. Due to the enormous length of blood vessels – more than 96,000 km in adult huma body oorganismu člověka – the total number of endothelial cells in the human body can reach numbers 10-60 billions cells.
In addition to transport of oxygen and nutrients toward the tissues, endothelial cells play lots of other functions. In embryonic development, before blood vessels are formed, a close contact between endothelial cells and developing cells of the liver or pancreas primordia is very important for tissue growth. Endothelial cells represent one of the elements of the stem cell niche – by producing specific factors (e.g., BDNF) they control stem cell behaviour.
MARKERS OF ENDOTHELIAL CELLS
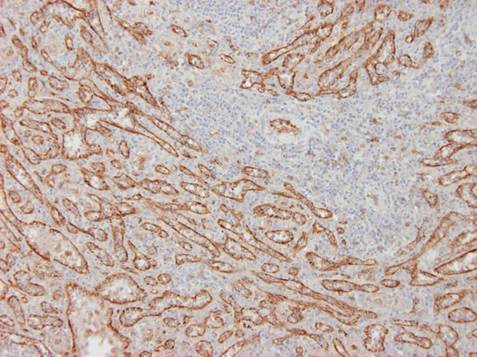
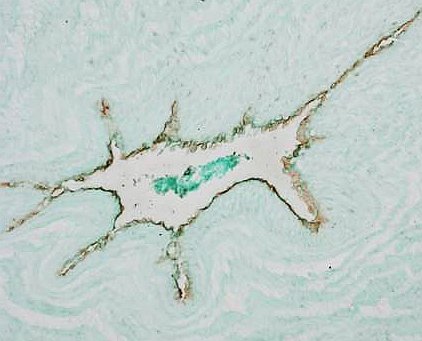
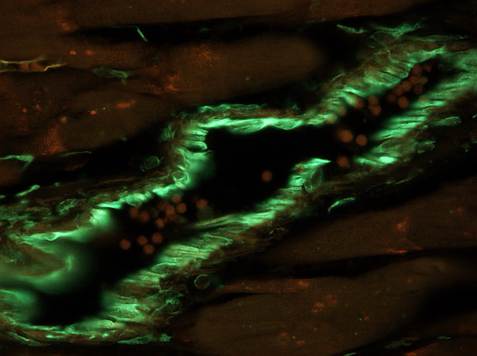
Typical markers of endothelial cells are: von Willebrand factor (Fig. 1A), CD34 (type 2), VE (vascular endothelial) cadherin, Tie2, KDR (VEGFR-2). However, there exists a phenotypic overlap between monocytes and mature vascular endothelial cells. Some markers used in endothelial detection, e.g. CD31 (PECAM), CD105 (endoglin) can be expressed by other cell types, e.g. monocytes/macrophages, and vice versa markers of macrophages, e.g. CD68 can be sometimes expressed by endothelial cells. For that reason none of the above mentioned markers is specific for endothelium only. Membranous glycoproteins can be distinguished with immunohistochemistry; polysaccharide components of endothelial cell glycocalyx can be detected with lectin histochemistry, e.g. Ulex europaeus I agglutinin (UEA-1) binds with high affinity to activated endothelial cells (e.g. in growing tumours, see Fig. 1B). Physiological approach for detection of live endothelial cells (e.g. cultured in vitro) is their uptake acetylated-LDL labelled with fluorochrome DiI (DiI-Ac-LDL uptake) although the same component can be also taken up by other cells, e.g. synovialocytes.
 |
 |
 |
| Fig. 1 A. Immunoperoxidase detection of von Willebrand factor in the spleen. Reaction reveals the lining of venous sinusoids inside of the red pulp. Counterstained with haematoxylin.
Author of the microfotograph: Jaroslav Mokrý. |
Fig. 1 B. UEA-1 lectin histochemistry. Reaction shows endothelial cells of blood vessels; to increase the intesity of the staining the reaction was amplified with biotinylated thyramin.
Author of the microfotograph: Jaroslav Mokrý. |
Fig. 1 C. Immunofluorescent detection of vimentin. Endothelial cells like other mesenchymal cells contain vimentin (green); detection identified the endothelium of muscular artery.
Author of the microfotograph: Jaroslav Mokrý. |
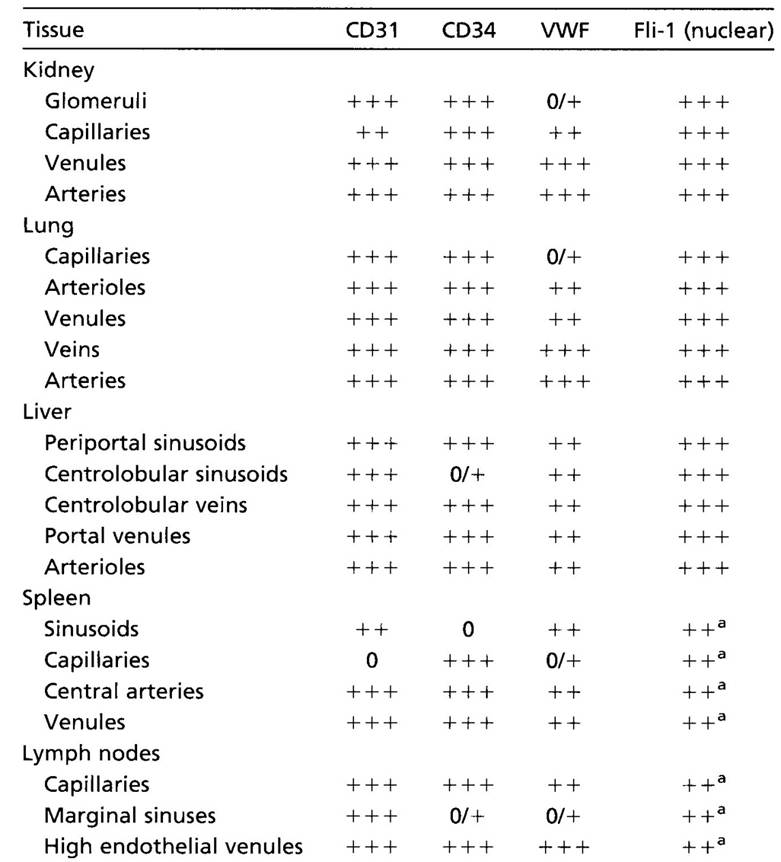
Endothelial cells are very heterogenic population. Different types of capillaries and vessels are lined with endothelium that expresses different markers: Ephrin-B3 is expressed in endothelial cells of arteries; Ephrin-B4, COUP-TFII in endothelium of veins; endothelium of lymphatic vessels express Lyve-1, Prox-1, VEGFR-3, podoplanin, and D2-40. Endothelial cells of tumours resemble activated cells and bear other markers, e.g. Tie-1,-2, VEGFR-2 and some integrins. Endothelium of haematoencephalic barrier is completely distinct by different properties and markers.
 |
||
| Tab. 1. Heterogeneity of endothelial cells. Expression of selected markers depends on the tissue and type of the blood vessel. |
